Human Papillomavirus (HPV) is a collective name for a group of DNA viruses that are transmitted from person to person and cause the development of benign neoplasms: papillomas. Some varieties are oncogenic (that is, they increase the risk of malignant tumors). HPV is most commonly associated with cervical cancer, which kills thousands of women worldwide each year. However, these viruses also affect the development of other cancers: not only in women, but also in men.
HPV does not manifest as symptoms for a long time - patients often discover it only when precancerous conditions or cancer develop. HPV is a threat to patients of any gender and age, including young children. But even so, their main "target audience" is people between the ages of 15 and 30 - they are sexually active, they don't always think about precautions, and in most cases, HPV is transmitted sexually.
To prevent the impact of the virus on the body from reaching so far, it is recommended to periodically monitor your health: to exclude pathologies that it may cause. There are also HPV tests to detect the presence of oncogenic strains. Take care of your health right now: make an appointment at the Otradnoe Polyclinic and go to a doctor's office without having to queue or adjust to an inconvenient schedule for you
What is HPV?
Human papillomaviruses, which enter the body through microtraumas of the skin, enter the cells of the basal layer of the epithelium. HPV can exist in any layer of the epidermis. However, its reproduction occurs exclusively in the basal layer.
The development of the virus occurs in 2 stages:
- Reproductive: the virus enters the cell without affecting its chromosomes and multiplies.
- Integrative: HPV is introduced into the genome of an infected cell.
It is during the second stage that the virus transforms cells. They begin to actively divide, and tumor formations (papillomas) appear. These are papillary growths that protrude above the surface of the skin (that's why they are called: papilloma - from Latin papilla - nipple and Greek oma - tumor). The second stage doesn't always happen. The virus, being in the first stage of development, can regress (leave the body). However, even if the patient does not have pathological changes, he is a carrier of HPV and can infect other people.
The incubation period can last from 3 weeks to a year. On average, it is 3 months. In some cases, non-genital forms of papillomas appear first and then neoplasms appear on the genitals.

In most cases, the body is faced with the virus within 2 years. However, reinfection can occur, with the same strain or with a different one. In addition, papillomas or other skin manifestations may regress after 6-8 months (they gradually decrease and then disappear). This happens when the immune system suppresses the virus and "survives" it from the cells.
The HPV virus most commonly affects the skin and mucous membranes:
- Anogenital area.
- Upper respiratory tract.
- Oral cavity.
- Bronchus.
- Conjunctiva.
- Straight.
- Esophagus.
Types of HPV
The first human papillomavirus (HPV) was isolated in 1971. And scientist Harald zur Hausen was able to identify and prove the connection between HPV and cervical cancer. Later, he received the Nobel Prize for his discoveries.
Currently about 600 different strains of HPV are known. Some cause the appearance of warts, others, genital warts and others, papillomas. There are also types of HPV that affect the development of cancerous tumors. They are called oncogenic. Fortunately, there are not many. They can have a low, medium or high oncogenic potential:
- Strains 6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81 are characterized by low oncogenicity.
- Average oncogenicity in types 26, 31, 33, 35, 51, 52, 53, 58, 66.
- High oncogenic potential in strains 16, 18, 39, 45, 56, 59, 68, 73, 82.
Cervical cancer is mainly caused by types 16 and 18.
Help!The presence of an oncogenic type of HPV in the body does not mean that a person is "doomed" to cancer. The presence of the virus increases the risk of developing cancer, but it is not the only cause of its appearance.If a patient has an oncogenic strain of HPV, he only needs to closely monitor her health and undergo regular preventive examinations. If necessary, the doctor will prescribe the appropriate therapy.
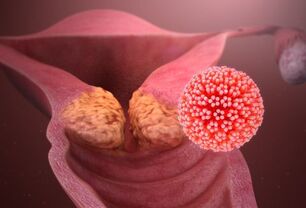
The reproductive system of women and men is capable of infecting around 40 types of papillomavirus. The result of its activity is not only cancer, but also genital warts or condylomas.
Help!Cancerous tumors develop slowly - 5 to 30 years after infection with the papilloma virus. They are preceded by precancerous conditions (benign neoplasms that can degenerate into malignant ones). That is why it is so important to get regular preventive exams. And precancerous conditions, and even cancer in the initial stages, are perfectly treatable and dangerous consequences can be avoided.
Routes of HPV transmission
The main "condition" of infection is the presence of microdamages (wounds, cracks, scrapes) on the skin or mucous membranes. They are the "doors" of HPV.
The most common transmission of the virus occurs when the skin or mucous membranes of two people come into contact. Therefore, the main route of papillomaviruses is sexual contact. Also, the use of condoms does not exclude the possibility of infection. The virus can be transmitted through oral sex, during which contraception is not always used. Also, the condom does not cover the entire surface of the penis and is often placed in the middle of intercourse. You can also get HPV by kissing.
HPV can also be transmitted:
- From mother to child as the baby passes through the birth canal.
- At home: when using other people's hygiene products (towels, toothbrushes, shaving accessories).
- In public places: saunas, gyms, swimming pools.
Help!The survival time of papillomaviruses in the external environment is short. Therefore, the risk of domestic contagion, although it exists, is much lower than with sexual contact.
Self-infection is also possible: the transfer of the virus from one part of the body to another during waxing, combing, biting nails.
Infection by contact with a virus does not occur in all cases. The following factors increase the risk:
- Decreased immunity.
- Bad habits: smoking, alcohol abuse.
- Stress.
- Sexually transmitted infections.
- Diseases of the urinary system.
- Lesions on the skin and mucous membranes.
- Immunodeficiency states.
- Long-term use of hormonal contraceptives.
Help!Oncogenic strains of HPV are more dangerous for women than men, as they are infected with them more often.
HPV: symptoms
Papillomaviruses are capable of not presenting any symptoms for a long time. Usually, the patient learns about the presence of HPV already with the development of its consequences: the appearance of warts, papillomas, condylomas. In some cases, the following signs may indicate the presence of a virus:
- Redness, skin growths (most often in the genital area);
- Itching.
- Pain and other discomfort during or after intercourse.
What diseases can HPV cause?
Papillomaviruses first cause the growth of papillomas, warts and genital warts in patients of both sexes. All of the above neoplasms can occur anywhere on the body. However, they most often affect the genitalia and anal region. In women, they occur on the vulva, cervix, and vagina. In men: the scrotum, the head of the penis, the foreskin. In patients of both sexes, neoplasms usually appear in the anus.
In addition, warts often appear on the soles of the feet, the larynx, and the vocal cords. Papillomas (flesh-colored papillomas) do not have a "favorite place"; They can appear on the trunk, neck, face, arms, and legs. In children and adolescents, flat warts are the most common (they are also called juvenile or juvenile). These are small dark neoplasms (3-5 mm) that protrude slightly above the surface of the skin. Most of the time they occur on the back of the hands, face, and legs.
As for cancer, most patients are associated with HPV, first of all cervical cancer. In fact, this pathology is very common in our time. However, in women, HPV also often causes the development of vaginal and vulvar cancer (65-70% of cases), in men - penile cancer (50% of cases). In addition, in both women and men, papillomaviruses can contribute to the development of malignant tumors:
- straight;
- oral cavity;
- larynx.
In children, HPV, as a rule, manifests itself by the growth of papillomas against the background of a decrease in immunity due to previous diseases, usually viral or bacterial infections. Additionally, papilloma viruses infect young patients who suffer from frequent colds or allergic reactions.
HPV and pregnancy
Papillomaviruses negatively affect female fertility. If they are present, the chance of pregnancy is cut in half, as HPV can interfere with the implantation of a fertilized egg. If the partner is also infected with the virus (which occurs in 65-70% of cases), the chance of conception decreases even more. HPV has a negative effect on the motility of sperm.
When pregnancy occurs, the papilloma virus increases the risk of developing:
- Little or polyhydramnios.
- Chronic placental insufficiency.
- HPV can also cause a miscarriage.
Therefore, pregnant women are prescribed a moderate drug treatment, which can significantly reduce all the above risks.
When a child passes through the birth canal, there is a risk of infection. Therefore, it is preferable for women with HPV to deliver by cesarean section; the risk of virus transmission is reduced by 5 times.
Changes in hormone levels cause rapid growth of genital warts. They can grow together, which can cause difficulties in the acts of urination and defecation, produce unpleasant sensations when walking, bleeding. During childbirth, neoplasms are easily injured. They can also make it difficult for the baby to pass through the birth canal. To avoid all of this, genital warts are treated early in pregnancy. Methods such as cryodestruction, laser surgery, etc. are used.
Diagnosis

To diagnose HPV, they first consult a doctor. Depending on the manifestations of the virus, he will refer the patient to diagnostic studies and to a narrow specialist (gynecologist, urologist, dermatologist, oncologist, proctologist, etc. ).
Exams can be assigned to men and women, such as:
- ELISA blood test: according to its results, it is impossible to determine the concentration and oncogenicity of the virus, but antibodies can be detected, the method is ideal for early diagnosis, when symptoms have not yet appeared.
- PCR Diagnostics - allows you to detect HPV DNA, that is, it lets you know exactly whether there is a virus in the body or not; blood, saliva, secretions from the genitals, etc. are taken. for your analysis.
- Digene-test: allows you to evaluate the degree of oncogenicity of a strain to establish the amount of virus in the body; biomaterial is a piece of tissue that is scraped from the cervical canal, vagina, or urethra.
Women are prescribed the following types of exams:
- Cytological examination (PAP test): Examination of a smear from the vagina under a microscope to identify cells altered by the virus.
- Colposcopy: examination of the cervix with a colposcope; This procedure is prescribed to the patient if altered cells are found according to the results of the cytological examination.
Treatment
There is no specific treatment for HPV (that is, intended to destroy it). However, you can take steps to suppress the activity of the virus and increase the likelihood of self-healing. The patient is prescribed:
- Vitamins.
- Immunomodulators.
- Antiviral drugs.
A symptomatic treatment is also carried out: elimination of neoplasms. In no case should you try to treat condylomas, papillomas and warts with folk remedies. There is a risk of causing the development of a secondary infection or the degeneration of a benign tumor into a malignant one.
The following methods are used to remove neoplasms:
- Scalpel removal.
- Cryodestruction (freezing with liquid nitrogen).
- Retreat with a radio knife.
- Laser removal.
- Electrocoagulation.
The physician chooses the method based on the nature and location of the neoplasm, as well as the condition of the patient's body.
Prevention

Preventive methods include maintaining a healthy lifestyle and regular strengthening of immunity with the help of a complete and varied diet, moderate physical activity, and quality rest. It is important to follow the rules of personal hygiene, not to use other people's accessories. To avoid the risk of infection, you must abstain from casual sex and use a barrier method of contraception.
Also today there is the possibility of vaccination against some highly oncogenic strains of HPV. Vaccinations are recommended between the ages of 9 and 26 (the optimal age is 11 to 12 years). Women can be vaccinated after age 26, but only if the gynecologist believes there is evidence. It should be noted that vaccination does not cure a virus already present in the body, but it does prevent infection with some of its especially dangerous types.























